Last Updated on: September 11, 2024
Table of Content:
One of the basic BLS tools, an oropharyngeal airway, considerably improves airway management during emergencies. The device prevents the tongue from obstructing the airway in unconscious patients, thereby allowing oxygen to pass through the lungs clearly.
In this regard, health professionals and BLS responders should develop competency in sizing, inserting, and managing oropharyngeal airways to facilitate the provision of optimum care in each patient and at every life-threatening situation. The article discusses the meaning and importance of OPA. It also details how to use this device and when to look for alternative options.
The oral airway device should be used only after a careful examination of the patient. The main indications for the use of the OPA are as follows:
An understanding of these indications is important for any healthcare professional and a BLS responder in the decision to use an oropharyngeal airway.
While OPAs are very helpful devices, there are some situations when their use is relatively or absolutely contraindicated. It is important to identify such contraindications to avoid potential harm to the patient. Let’s take a look at which is a contraindication to the use of an oropharyngeal airway:
Read More: How do you perform CPR on a drowned person?
Appropriate size of OPA should be chosen for best effects and avoidance of possible complications. Oral airway measurement is quite simple, but attention needs to be given to details:
The first item of relevance to determining the right size OPA is a measurement from the patient’s mouth corner to either one of the two following body points: angle of the jaw or earlobe. The anatomy of the oral cavity and pharynx is approximately proportional to this external facial measurement.
This distance can be measured using a ruler or the OPA itself. The patient’s head should be in a neutral position while measuring.
After the rough measurement, the real OPA must be inserted for a measurement. Hold the OPA against the side of the patient’s face, positioning the flange (the wider, outer part) at the corner of the mouth. The tip of the OPA should reach the angle of the jaw or the earlobe without extending beyond it.
If it’s too long, it could cause airway obstruction or stimulate the gag reflex. If it’s too short, it won’t effectively hold the tongue off the back of the pharynx.
OPAs typically come in standardized, numbered sizes:
Adult OPAs usually range from 80mm to 120mm in length. Each size increment typically represents a 10mm increase in length.
Size guide:
Pediatric sizes are smaller, typically ranging from 30mm to 70mm.
Even though the estimations are a useful tool, specific patient anatomy must also be considered. Some factors that may justify a change in size are:
This is because, in some patients, a size different from what the initial measurement dictates may be needed. Always be prepared to reassess and adjust as needed.
When in doubt between two sizes, it’s generally safer to choose the smaller size. A slightly smaller OPA is less likely to cause complications than one that’s too large. Even though it’s slightly smaller, it can still be effective in maintaining the airway and poses less risk of complications.
Oropharyngeal airway insertion is one of the most significant skills in airway management. This procedure involves attention to detail and should be well understood in terms of the technique for its execution to ensure the safety of the patient and the effectiveness of airway maintenance.
To start with, the oropharyngeal airway requires assessment of the patient. Assess for unconsciousness and absence of gag reflex. This assessment is crucial because inserting an OPA in a conscious patient or a patient with an intact gag reflex can lead to complications such as vomiting or laryngospasm. Assess consciousness by trying to arouse the patient verbally and by gentle physical stimulation.
Once you have determined that an OPA is appropriate, choose the right size. Measuring techniques, as discussed earlier, include from the corner of the mouth to the angle of the jaw or the earlobe. A correctly fitted OPA would run from the patient’s central incisors to just above the jaw angle.
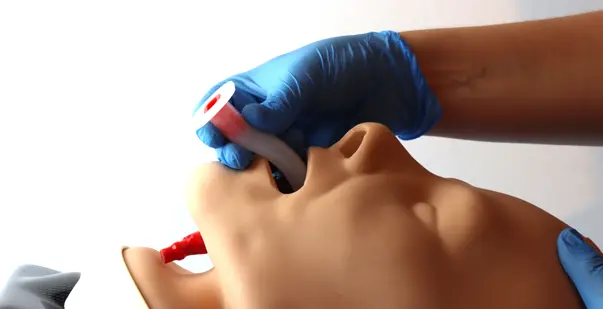
To safely insert an OPA, you will need clear access to the oral cavity. Open the patient’s mouth gently but firmly using the cross-finger technique.
This technique involves placing your thumb on the lower teeth and your index finger on the upper teeth, applying gentle pressure in opposite directions. Be cautious not to use excessive force, especially if dental injuries are suspected.
The insertion technique is slightly different for adults and children:
First and foremost, select the first step in the use of an oropharyngeal airway. This includes opening the mouth. Then, the OPA is introduced upside down with the curved end directed towards the roof of the mouth. This orientation avoids forcing the tongue backward.
A key aspect of insertion is to confirm the proper oral airway placement. The flange must rest comfortably outside the mouth, and the airway curve is supposed to follow the roof of the mouth, with the tip lying just above the epiglottis. Improper placement results in obstruction of the airway or inefficient ventilation.
Once the OPA is in place, check for its effectiveness by looking for chest rise with ventilation and listening for air movement. If you are using bag-mask ventilation, you should be able to provide breaths without difficulty.
If these breaths are resistant or the chest rise is poor, the position of the OPA should once again be reassessed. If it remains ineffective, the airway adjunct may need to be either repositioned or replaced.
Although OPAs generally do not require additional securing devices, they must stay in place. Check regularly to ensure the OPA has not been dislodged during patient movement or transport. If the OPA is considered unstable, consider reviewing its size and placement.
Read more: Hospital Emergency Codes: Part 1 – Universal Codes
Once an OPA is in place, ongoing care and assessment is crucially important:
Thus, you should always stay updated with appropriate training to grasp a better understanding of procedures involving the oropharyngeal airway in BLS.
The oropharyngeal airway is an important tool in Basic Life Support procedures. It can change the outcome of a medical condition during emergencies. As a healthcare provider, you must understand the first step while using an oropharyngeal airway. It helps in handling patients experiencing respiratory problems.
Remember that incorporating the OPA into BLS protocols can improve patient outcomes. However, proper device placement and mishandling issues should be addressed to avoid complications. If done properly, OPA can help resolve breathing difficulty and save the patient.