Last Updated on: September 2, 2024
Table Of Content(s)
Every two hours, a youngster in the United States goes into cardiac arrest. This truth emphasizes the great value of Child BLS (Basic Life Support) knowledge. With approximately 4 out of 5 cardiac arrests occurring at home, often witnessed by family members, the knowledge of pediatric resuscitation techniques becomes invaluable.
Schools that include BLS instruction in their courses have shown a notable rise in bystander CPR performance, therefore possibly saving many young lives. Mastery of these skills may turn ordinary people into lifesavers.
Are you ready to take on the skill to protect a child’s most valuable gift—their life? Let us explore the field of pediatric resuscitation and release the ability to transform a life.
Child BLS is the fundamental life-saving skill applied to children between the ages of one and puberty. It includes a series of vital movements meant to promote circulation and respiration during an emergency. Child BLS, unlike adult BLS, needs particular adaptations because of the unique anatomy and physiology of children.
A fast response may greatly raise survival rates in pediatric crises. Good procedures can preserve important organ function until expert assistance arrives.
Key differences in Child BLS include gentler chest compressions and a different child rescue breathing rate. For children, rescuers should aim for 15-20 breaths per minute, compared to 10-12 for adults. Hand placement and compression depth also vary based on the child’s size.
Anyone caring for children must understand these differences. Learning Child BLS helps people respond quickly and powerfully to crucial events that can save young lives.
Rapid detection of pediatric crises is crucial for prompt response. Acting fast and knowing the symptoms might help save a life. Let’s explore typical situations and their obvious indicators.
A young kid can abruptly stop speaking, grasp their throat, or show scared facial expressions. As they battle to breathe, their face might become red or blue. These times call for quick action. Choking can rapidly progress from mild to severe, potentially leading to unconsciousness if not addressed promptly.
In drowning situations, a child could be found unresponsive in or near water. Their skin might seem blue or pale, and they could not be breathing or have a weak pulse. Consider “secondary drowning” symptoms even after rescue. These might show up hours after the event and include coughing constantly, chest discomfort, trouble breathing, or excessive tiredness. Since these delayed signs may point to major consequences, constant observation is very important.
Rare in children, cardiac arrest calls for quick response. A youngster can pass out, lose consciousness, and cease breathing all of a sudden. Initiating Child BLS depends on early recognition of these symptoms.
Saving a child’s life may depend on the recognition of the signs indicating the need for child BLS. Early and quick detection of symptoms such as:
Look for labored breathing, nostril flaring, or chest retractions. Young children may breathe using supplementary muscles or produce odd breathing noises like grunting or wheezing. These symptoms point to major respiratory problems needing quick care.
Look for pale or blue skin, especially around the lips and nail beds. Weak pulse, chilly extremities, or diminished responsiveness indicate impaired circulation. Severe instances might cause a youngster to become unconscious or sluggish.
Bluish coloring of the lips, tongue, or nail beds (cyanosis) points to a blood oxygen deficiency. Conversely, severe paleness or a grayish skin tone might also indicate inadequate circulation. These color shifts, particularly when combined with chilly, clammy skin, point to the child’s body not receiving enough oxygen, maybe from cardiac or respiratory issues.
Read More: CPR Ratio for Adults, Children, and Infants
Ensuring scene safety comes first, even before going to assist a child with stress. A safe atmosphere safeguards both the rescuer and the kid from future injury. You create the conditions for successful intervention by pausing to evaluate and protect the situation. Let’s explore the crucial steps in what are the correct actions to take for scene safety and assessment.
Tap or gently shake the child. With a light touch, see if the child moves or makes any noise. If there is no response, loudly call out to the child, asking if they are okay.
Gently place the child on their back on a firm, flat surface. If you believe the child has a spinal injury, move them only if absolutely required. In such cases, preferably, two people should gently move the youngster while keeping spinal alignment. Accurate evaluation and successful CPR, if necessary, depend on this correct posture. Remember, correct placement sets the foundation for all subsequent steps in the Child BLS process.
Spend no more than ten seconds looking, listening, and feeling for breathing. Start CPR if the kid is gasping or not breathing. For older children, feel at the carotid artery; for newborns, feel at the brachial artery. Start CPR right away if there is no pulse.
Basic Life Support (BLS) for a child requires a certain set of procedures. We will walk you through the key BLS algorithm child stages so you are ready to respond quickly and powerfully in an emergency. Recall that these methods are meant for children ranging in age from one year to adolescence.
Look for any risks like electrical problems, fire, or traffic. If you witnessed the collapse of a child, quickly assess the surroundings. Your safety comes first; you cannot assist if you become a victim yourself. Confirm the situation is safe, and then gently approach the child. Good intervention is built up by this first evaluation.
Ask the youngster loudly, “Are you okay?” after lightly tapping their shoulder. The infant BLS algorithm advises flicking the bottom of their feet for newborns. If there’s no response, it is confirmed that the child is unresponsive. Moreover, if a child is unresponsive, what is the next step in BLS in such cases? You should check for breathing and call for help. Determining the child’s degree of awareness and directing your next activities depends on this phase, which is very important.
If the child is unresponsive, the next step BLS is to call for emergency services immediately. If you’re alone and didn’t witness the collapse, perform 2 minutes of CPR before calling for help. Clearly describe your location and the circumstances when you call. As you start treatment, put the phone on speaker or get a bystander to call. The child’s chances of survival will be enhanced with quick expert treatment.
Head-tilt chin-lift is the technique to open the airways. Holding one hand on the child’s forehead, gently tilt the head back. Lift the chin to open the airway with your other hand. Babies should have a neutral head posture and only raise their chin. In the BLS algorithm child, this stage is crucial as it guarantees a free channel for air to reach the lungs.
Look for chest rise and fall, listen for breath sounds, and feel for air from the nose or mouth. Take no longer than 10 seconds to assess if the youngster is breathing regularly. Prepare to begin rescue breaths if the child is not breathing or is only gasping. Recall that in pediatric situations, respiratory difficulties usually precede cardiac problems; hence, this step is very important.
Start rescue breaths straight away if the youngster is not breathing properly. Pinch the nose tight and make a seal with yours over a child’s mouth. Cover the mouth and nose of a newborn with your mouth. Give two rescue breaths, each lasting approximately a second and strong enough to raise the chest. As mentioned earlier, the child rescue breathing rate should be about 12-20 breaths per minute. If the chest does not lift, adjust the head and try once again. Effective rescue breaths are essential for oxygenating the child’s body; sometimes, they are sufficient for regular breathing to resume.
Read More: Why is BLS Certification Required for an Emergency Medical Team Member?
Evaluating an unresponsive person depends critically on doing a pulse check. This process guides decisions on whether CPR is required. If the child is unresponsive after you tap his shoulders and shout, the next step in child BLS is to check for breathing and pulse. Let’s break down the parts of an effective pulse check.
Start by laying the victim back on a hard, level surface. This posture allows appropriate examination and CPR. Then, fast-check for breathing by feeling for air from the nose or mouth, hearing for breath sounds, and noting chest movement. For this part, take no more than ten seconds.
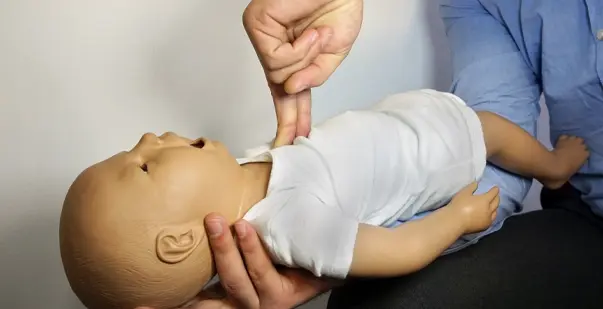
In newborns, look for the brachial pulse on the inside side of the upper arm, between the shoulder and elbow. Children’s carotid pulse may be found in the neck’s groove next to the trachea. To prevent mistaking your pulse for the victim’s, use two fingers.
Feel for the pulse for at least 5 seconds but no more than 10. If you fail to find a pulse during this period, start CPR immediately. If a pulse is detected, keep an eye on the person and, if rescue breaths are required, provide them until emergency services show up.
Even for children, automated external defibrillators (AEDs) are extremely important instruments for resuscitation attempts. Although adults and children utilize AED for similar fundamental purposes, there are significant distinctions to take into account. Knowing these differences can improve the results of cardiac crises in children.
When a child becomes unresponsive and does not breathe properly, an AED should be utilized as soon as it is accessible. Don’t delay CPR waiting for an AED, but apply it immediately once it arrives. Designed to examine the cardiac rhythm, AEDs only shock the patient if absolutely needed. Learning AED usage through a reputable course and applying it in situations of abrupt cardiac arrest may help even young children.
If available, use pediatric pads for youngsters under eight years old or weighing less than 55 pounds (25 kg). Lay one pad on the back’s center and the other on the chest’s center. If pediatric pads are not available, adult pads may be utilized. For older children, follow adult pad placement: one pad on the upper right chest and the other on the lower left side of the chest.
Ensure the child is not lying on a metal surface or in water. Eliminate any jewelry or prescription patches that might impede pad insertion. For small children, pick the pediatric setting if using an AED with an energy dosage selector. When the AED is evaluating or giving a shock, always follow its voice instructions and make sure nobody else is handling the kid. After the shock, or if no shock is advised, immediately resume CPR.
Learning child BLS skills is not only an advantage but also a duty for everyone who deals with children. These skills are not just beneficial; they are essential for protecting young lives in emergencies. Child BLS equips you with the knowledge to perform age-appropriate CPR, use an AED safely on children, respond to choking incidents, and assess and manage pediatric emergencies.
Being BLS trained provides you with the skills to act confidently in critical situations. Perhaps your skill, coupled with preparedness, will save a child’s life. Your investment in Child BLS training today can help you protect the children within your care and those around you.